-
Couser, W. G. Primary membranous nephropathy. Clin. J. Am. Soc. Nephrol. 12, 983–997 (2017).
CAS PubMed PubMed Central Google Scholar
-
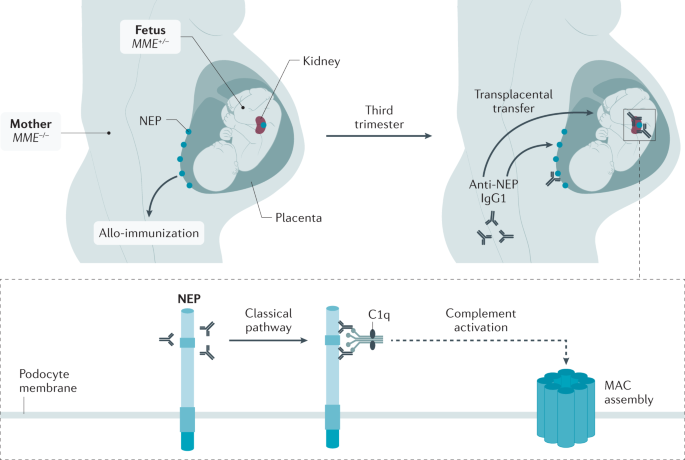
Debiec, H. et al. Antenatal membranous glomerulonephritis due to anti-neutral endopeptidase antibodies. N. Engl. J. Med. 346, 2053–2060 (2002). A landmark article that reports the first description of a podocyte antigen involved in a rare subset of neonatal MN.
PubMed Google Scholar
-
Beck, L. H. et al. M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N. Engl. J. Med. 361, 11–21 (2009). A landmark article that first characterizes the major antigen in adult MN, leading to a paradigm shift in the diagnosis and monitoring of patients.
CAS PubMed PubMed Central Google Scholar
-
Tomas, N. M. et al. Thrombospondin type-1 domain-containing 7A in idiopathic membranous nephropathy. N. Engl. J. Med. 371, 2277–2287 (2014). The first report of an antigen found to be associated with cancer in a subset of patients.
PubMed PubMed Central Google Scholar
-
Ronco, P. & Debiec, H. Membranous nephropathy: current understanding of various causes in light of new target antigens. Curr. Opin. Nephrol. Hypertens. 30, 287–293 (2021).
CAS PubMed PubMed Central Google Scholar
-
Sethi, S. New ‘antigens’ in membranous nephropathy. J. Am. Soc. Nephrol. 32, 268–278 (2021).
CAS PubMed Google Scholar
-
Cattran, D. C. & Brenchley, P. E. Membranous nephropathy: integrating basic science into improved clinical management. Kidney Int. 91, 566–574 (2017).
CAS PubMed Google Scholar
-
Dahan, K. et al. Rituximab for severe membranous nephropathy: a 6-month trial with extended follow-up. J. Am. Soc. Nephrol. 28, 348–358 (2017).
CAS PubMed Google Scholar
-
Fervenza, F. C. et al. Rituximab or cyclosporine in the treatment of membranous nephropathy. N. Engl. J. Med. 381, 36–46 (2019). This landmark randomized clinical trial provides the first comparison of rituximab and cyclosporine.
CAS PubMed Google Scholar
-
Fernández-Juárez, G. et al. The STARMEN trial indicates that alternating treatment with corticosteroids and cyclophosphamide is superior to sequential treatment with tacrolimus and rituximab in primary membranous nephropathy. Kidney Int. 99, 986–998 (2021). This important randomized clinical trial provides the first comparison of cyclophosphamide (with corticosteroids) with a sequential combination of tacrolimus and rituximab.
PubMed Google Scholar
-
Scolari, F. et al. Rituximab or cyclosphamide in the treatment of membranous nephropathy. J. Am. Soc. Nephrol. 32, 972–982 (2021).
CAS PubMed Central Google Scholar
-
De Vriese, A. S., Glassock, R. J., Nath, K. A., Sethi, S. & Fervenza, F. C. A proposal for a serology-based approach to membranous nephropathy. J. Am. Soc. Nephrol. 28, 421–430 (2017).
PubMed Google Scholar
-
Kumar, V. et al. Antibodies to m-type phospholipase A2 receptor in children with idiopathic membranous nephropathy. Nephrology 20, 572–575 (2015).
CAS PubMed Google Scholar
-
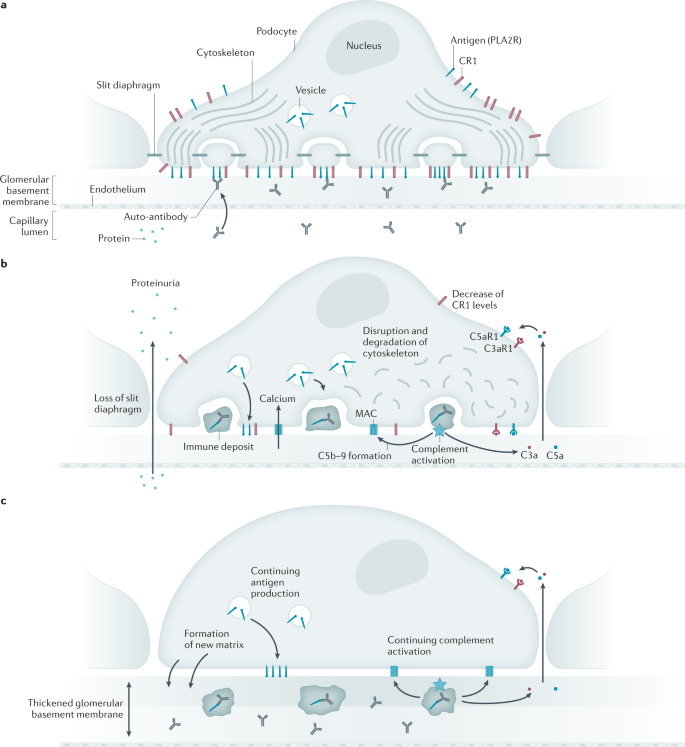
Debiec, H. & Ronco, P. Immunopathogenesis of membranous nephropathy: an update. Semin. Immunopathol. 36, 381–397 (2014).
CAS PubMed Google Scholar
-
McGrogan, A., Franssen, C. F. & de Vries, C. S. The incidence of primary glomerulonephritis worldwide: a systematic review of the literature. Nephrol. Dial. Transplant. 26, 414–430 (2011).
PubMed Google Scholar
-
Rychlik, I. et al. The Czech registry of renal biopsies. Occurrence of renal diseases in the years 1994-2000. Nephrol. Dial. Transplant. 19, 3040–3049 (2004).
PubMed Google Scholar
-
Hogan, S. L., Muller, K. E., Jennette, J. C. & Falk, R. J. A review of therapeutic studies of idiopathic membranous glomerulopathy. Am. J. Kidney Dis. 25, 862–875 (1995).
CAS PubMed Google Scholar
-
Xu, X. et al. Long-term exposure to air pollution and increased risk of membranous nephropathy in China. J. Am. Soc. Nephrol. 27, 3739–3746 (2016).
CAS PubMed PubMed Central Google Scholar
-
Ronco, P. & Debiec, H. Pathophysiological advances in membranous nephropathy: time for a shift in patient’s care. Lancet 385, 1983–1992 (2015).
PubMed Google Scholar
-
Arapovic, A. et al. Epidemiology of 10-year paediatric renal biopsies in the region of southern Croatia. BMC Nephrol. 21, 65 (2020).
CAS PubMed PubMed Central Google Scholar
-
Chen, A. et al. Idiopathic membranous nephropathy in pediatric patients: presentation, response to therapy, and long-term outcome. BMC Nephrol. 8, 11 (2007).
PubMed PubMed Central Google Scholar
-
Eddy, A. A. & Symons, J. M. Nephrotic syndrome in childhood. Lancet 362, 629–639 (2003).
PubMed Google Scholar
-
Nie, S. et al. The spectrum of biopsy-proven glomerular diseases among children in China: a national, cross-sectional survey. Clin. J. Am. Soc. Nephrol. 13, 1047–1054 (2018).
PubMed PubMed Central Google Scholar
-
Johnson, R. J. & Couser, W. G. Hepatitis B infection and renal disease: clinical, immunopathogenetic and therapeutic considerations. Kidney Int. 37, 663–676 (1990).
CAS PubMed Google Scholar
-
Moroni, G. & Ponticelli, C. Secondary membranous nephropathy. a narrative review. Front. Med. 7, 611317 (2020).
Google Scholar
-
Xu, X., Nie, S., Ding, H. & Hou, F. F. Environmental pollution and kidney diseases. Nat. Rev. Nephrol. 14, 313–324 (2018).
CAS PubMed Google Scholar
-
Narasimhan, B. et al. Characterization of kidney lesions in Indian adults: towards a renal biopsy registry. J. Nephrol. 19, 205–210 (2006).
PubMed Google Scholar
-
Li, J. et al. Primary glomerular nephropathy among hospitalized patients in a national database in China. Nephrol. Dial. Transpl. 33, 2173–2181 (2018).
CAS Google Scholar
-
Schieppati, A. et al. Prognosis of untreated patients with idiopathic membranous nephropathy. N. Engl. J. Med. 329, 85–89 (1993).
CAS PubMed Google Scholar
-
Ponticelli, C. et al. A 10-year follow-up of a randomized study with methylprednisolone and chlorambucil in membranous nephropathy. Kidney Int. 48, 1600–1604 (1995).
CAS PubMed Google Scholar
-
Jha, V. et al. A randomized, controlled trial of steroids and cyclophosphamide in adults with nephrotic syndrome caused by idiopathic membranous nephropathy. J. Am. Soc. Nephrol. 18, 1899–1904 (2007).
CAS PubMed Google Scholar
-
Maisonneuve, P. et al. Distribution of primary renal diseases leading to end-stage renal failure in the United States, Europe, and Australia/New Zealand: results from an international comparative study. Am. J. Kidney Dis. 35, 157–165 (2000).
CAS PubMed Google Scholar
-
Troyanov, S. et al. Idiopathic membranous nephropathy: definition and relevance of a partial remission. Kidney Int. 66, 1199–1205 (2004).
PubMed Google Scholar
-
Fervenza, F. C., Sethi, S. & Specks, U. Idiopathic membranous nephropathy: diagnosis and treatment. Clin. J. Am. Soc. Nephrol. 3, 905–919 (2008).
PubMed Google Scholar
-
Klouda, P. T. et al. Strong association between idiopathic membranous nephropathy and HLA-DRW3. Lancet 2, 770–771 (1979).
CAS PubMed Google Scholar
-
Vaughan, R. W., Demaine, A. G. & Welsh, K. I. A DQA1 allele is strongly associated with idiopathic membranous nephropathy. Tissue Antigens 34, 261–269 (1989).
CAS PubMed Google Scholar
-
Stanescu, H. C. et al. Risk HLA-DQA1 and PLA(2)R1 alleles in idiopathic membranous nephropathy. N. Engl. J. Med. 364, 616–626 (2011).
CAS PubMed Google Scholar
-
Coenen, M. J. et al. Phospholipase A2 receptor (PLA2R1) sequence variants in idiopathic membranous nephropathy. J. Am. Soc. Nephrol. 24, 677–683 (2013).
CAS PubMed PubMed Central Google Scholar
-
Lv, J. et al. Interaction between PLA2R1 and HLA-DQA1 variants associates with anti-PLA2R antibodies and membranous nephropathy. J. Am. Soc. Nephrol. 24, 1323–1329 (2013).
CAS PubMed PubMed Central Google Scholar
-
Le, W. B. et al. HLA-DRB1*15:01 and HLA-DRB3*02:02 in PLA2R-Related membranous nephropathy. J. Am. Soc. Nephrol. 28, 1642–1650 (2017).
CAS PubMed Google Scholar
-
Cui, Z. et al. MHC class II risk alleles and amino acid residues in idiopathic membranous nephropathy. J. Am. Soc. Nephrol. 28, 1651–1664 (2017).
CAS PubMed Google Scholar
-
Xie, J. et al. The genetic architecture of membranous nephropathy and its potential to improve non-invasive diagnosis. Nat. Commun. 11, 1600 (2020). The most extensive multi-ethnic genome-wide association study performed in membranous nephropathy revealing the complexity of HLA-D alleles associated with membranous nephropathy in different ethnic populations and signals in the NF-κB and interferon pathways.
CAS PubMed PubMed Central Google Scholar
-
Wang, H. Y. et al. HLA class II alleles differing by a single amino acid associate with clinical phenotype and outcome in patients with primary membranous nephropathy. Kidney Int. 94, 974–982 (2018).
CAS PubMed Google Scholar
-
Van Damme, B. J., Fleuren, G. J., Bakker, W. W., Vernier, R. L. & Hoedemaeker, P. J. Experimental glomerulonephritis in the rat induced by antibodies directed against tubular antigens. V. Fixed glomerular antigens in the pathogenesis of heterologous immune complex glomerulonephritis. Lab. Invest. 38, 502–510 (1978).
PubMed Google Scholar
-
Couser, W. G., Steinmuller, D. R., Stilmant, M. M., Salant, D. J. & Lowenstein, L. M. Experimental glomerulonephritis in the isolated perfused rat kidney. J. Clin. Invest. 62, 1275–1287 (1978).
CAS PubMed PubMed Central Google Scholar
-
Kerjaschki, D. & Farquhar, M. G. Immunocytochemical localization of the Heymann nephritis antigen (GP330) in glomerular epithelial cells of normal Lewis rats. J. Exp. Med. 157, 667–686 (1983).
CAS PubMed PubMed Central Google Scholar
-
Prabakaran, T. et al. Receptor-mediated endocytosis of α-galactosidase A in human podocytes in Fabry disease. PLoS ONE 6, e25065 (2011).
CAS PubMed PubMed Central Google Scholar
-
Debiec, H. et al. Role of truncating mutations in MME gene in feto-maternal allo-immunization and neonatal glomerulopathies. Lancet 364, 1252–1259 (2004).
CAS PubMed Google Scholar
-
Turner, A. J., Isaac, R. E. & Coates, D. The neprilysin (NEP) family of zinc metalloendopeptidases: genomics and function. Bioessays 23, 261–269 (2001).
CAS PubMed Google Scholar
-
Lu, B. et al. The control of microvascular permeability and blood pressure by neutral endopeptidase. Nat. Med. 3, 904–907 (1997).
CAS PubMed Google Scholar
-
Platt, J. L., Tucker, W. L. & Michael, A. F. Stages of renal ontogenesis identified by monoclonal antibodies reactive with lymphohematopoietic differentiation antigens. J. Exp. Med. 157, 155–172 (1983).
CAS PubMed Google Scholar
-
Vivarelli, M. et al. Genetic homogeneity but IgG subclass-dependent clinical variability of alloimmune membranous nephropathy with anti-neutral endopeptidase antibodies. Kidney Int. 87, 602–609 (2015).
PubMed Google Scholar
-
Hogan, M. C. et al. Subfractionation, characterization, and in-depth proteomic analysis of glomerular membrane vesicles in human urine. Kidney Int. 85, 1225–1237 (2014).
CAS PubMed Google Scholar
-
Ancian, P., Lambeau, G., Mattei, M. G. & Lazdunski, M. The human 180-kDa receptor for secretory phospholipases A2. Molecular cloning, identification of a secreted soluble form, expression, and chromosomal localization. J. Biol. Chem. 270, 8963–8970 (1995).
CAS PubMed Google Scholar
-
Fresquet, M. et al. Identification of a major epitope recognized by PLA2R autoantibodies in primary membranous nephropathy. J. Am. Soc. Nephrol. 26, 302–313 (2015).
PubMed Google Scholar
-
Seitz-Polski, B. et al. Epitope spreading of autoantibody response to PLA2R associates with poor prognosis in membranous nephropathy. J. Am. Soc. Nephrol. 27, 1517–1533 (2016).
CAS PubMed Google Scholar
-
Reinhard, L. et al. Clinical relevance of domain-specific phospholipase A2 receptor 1 antibody levels in patients with membranous nephropathy. J. Am. Soc. Nephrol. 31, 197–207 (2020).
CAS PubMed Google Scholar
-
Seitz-Polski, B. et al. Phospholipase A2 receptor 1 epitope spreading at baseline predicts reduced likelihood of remission of membranous nephropathy. J. Am. Soc. Nephrol. 29, 401–408 (2018).
CAS PubMed Google Scholar
-
Kanigicherla, D. et al. Anti-PLA2R antibodies measured by ELISA predict long-term outcome in a prevalent population of patients with idiopathic membranous nephropathy. Kidney Int. 83, 940–948 (2013).
CAS PubMed Google Scholar
-
Godel, M., Grahammer, F. & Huber, T. B. Thrombospondin type-1 domain-containing 7A in idiopathic membranous nephropathy. N. Engl. J. Med. 372, 1073 (2015).
PubMed Google Scholar
-
Herwig, J. et al. Thrombospondin type 1 domain-containing 7A localizes to the slit diaphragm and stabilizes membrane dynamics of fully differentiated podocytes. J. Am. Soc. Nephrol. 30, 824–839 (2019).
CAS PubMed PubMed Central Google Scholar
-
Seifert, L. et al. The most N-terminal region of THSD7A Is the predominant target for autoimmunity in THSD7A-associated membranous nephropathy. J. Am. Soc. Nephrol. 29, 1536–1548 (2018).
CAS PubMed PubMed Central Google Scholar
-
Hoxha, E. et al. A mechanism for cancer-associated membranous nephropathy. N. Engl. J. Med. 374, 1995–1996 (2016).
PubMed Google Scholar
-
Hoxha, E. et al. An indirect immunofluorescence method facilitates detection of thrombospondin type 1 domain-containing 7A-specific antibodies in membranous nephropathy. J. Am. Soc. Nephrol. 28, 520–531 (2017).
CAS PubMed Google Scholar
-
Sethi, S. et al. Exostosin 1/exostosin 2-associated membranous nephropathy. J. Am. Soc. Nephrol. 30, 1123–1136 (2019). This article reports the first use of a technological leap combining microdissection of glomeruli and mass spectrometry for the identification of the first biomarker of lupus membranous nephropathy.
CAS PubMed PubMed Central Google Scholar
-
Ravindran, A. et al. In patients with membranous lupus nephritis, exostosin-positivity and exostosin-negativity represent two different phenotypes. J. Am. Soc. Nephrol. 32, 695–706 (2021).
CAS PubMed PubMed Central Google Scholar
-
Saidi, M. et al. The exostosin immunohistochemical status differentiates lupus membranous nephropathy subsets with different outcomes. Kidney Int. Rep. 6, 1977–1980 (2021).
PubMed PubMed Central Google Scholar
-
Caza, T. et al. NELL1 is a target antigen in malignancy-associated membranous nephropathy. Kidney Int. 99, 967–976 (2021).
CAS PubMed Google Scholar
-
Sethi, S. et al. Neural epidermal growth factor-like 1 protein (NELL-1) associated membranous nephropathy. Kidney Int. 97, 163–174 (2020). This article reports the identification of the second prevalent antigen (after PLA2R) in MN using glomerular microdissection followed by mass spectrometry.
CAS PubMed Google Scholar
-
Kudose, S. et al. The clinicopathologic spectrum of segmental membranous glomerulopathy. Kidney Int. 99, 247–255 (2021).
CAS PubMed Google Scholar
-
Sethi, S. et al. Semaphorin 3B-associated membranous nephropathy is a distinct type of disease predominantly present in pediatric patients. Kidney Int. 98, 1253–1264 (2020).
CAS PubMed Google Scholar
-
Caza, T. et al. Neural cell adhesion molecule 1 is a novel autoantigen in membranous lupus nephritis. Kidney Int. 100, 171–181 (2021).
CAS PubMed Google Scholar
-
Sethi, S. et al. Protocadherin 7-associated Membranous Nephropathy. J. Am. Soc. Nephrol. 32, 1249–1261 (2021).
CAS PubMed PubMed Central Google Scholar
-
Al-Rabadi, L. F. et al. Serine protease HTRA1 as a novel target antigen in primary membranous nephropathy. J. Am. Soc. Nephrol. https://doi.org/10.1681/ASN.2020101395 (2021).
Article PubMed Google Scholar
-
Meyer-Schwesinger, C. et al. A novel mouse model of phospholipase A2 receptor 1-associated membranous nephropathy mimics podocyte injury in patients. Kidney Int. 97, 913–919 (2020).
CAS PubMed Google Scholar
-
Blosser, C. D., Ayalon, R., Nair, R., Thomas, C. & Beck, L. H. Jr. Very early recurrence of anti-Phospholipase A2 receptor-positive membranous nephropathy after transplantation. Am. J. Transplant. 12, 1637–1642 (2012).
CAS PubMed Google Scholar
-
Stahl, R., Hoxha, E. & Fechner, K. PLA2R autoantibodies and recurrent membranous nephropathy after transplantation. N. Engl. J. Med. 363, 496–498 (2010).
PubMed Google Scholar
-
Beck, L. H. Jr et al. Rituximab-induced depletion of anti-PLA2R autoantibodies predicts response in membranous nephropathy. J. Am. Soc. Nephrol. 22, 1543–1550 (2011).
CAS PubMed PubMed Central Google Scholar
-
Ruggenenti, P. et al. Anti-phospholipase A2 receptor antibody titer predicts post-rituximab outcome of membranous nephropathy. J. Am. Soc. Nephrol. 26, 2545–2558 (2015).
CAS PubMed PubMed Central Google Scholar
-
Debiec, H. et al. Early-childhood membranous nephropathy due to cationic bovine serum albumin. N. Engl. J. Med. 364, 2101–2110 (2011). A landmark article that identifies the first food antigen involved in rare cases of membranous nephropathy in children.
CAS PubMed Google Scholar
-
Border, W. A., Ward, H. J., Kamil, E. S. & Cohen, A. H. Induction of membranous nephropathy in rabbits by administration of an exogenous cationic antigen. J. Clin. Invest. 69, 451–461 (1982).
CAS PubMed PubMed Central Google Scholar
-
Adler, S. G., Wang, H., Ward, H. J., Cohen, A. H. & Border, W. A. Electrical charge. Its role in the pathogenesis and prevention of experimental membranous nephropathy in the rabbit. J. Clin. Invest. 71, 487–499 (1983).
CAS PubMed PubMed Central Google Scholar
-
Hunley, T. E. et al. Nephrotic syndrome complicating α-glucosidase replacement therapy for Pompe disease. Pediatrics 114, e532–e535 (2004).
PubMed Google Scholar
-
Debiec, H. et al. Allo-immune membranous nephropathy and recombinant aryl sulfatase replacement therapy: a need for tolerance induction therapy. J. Am. Soc. Nephrol. 25, 675–680 (2013).
PubMed PubMed Central Google Scholar
-
Burbelo, P. D. et al. Detection of PLA2R autoantibodies before the diagnosis of membranous nephropathy. J. Am. Soc. Nephrol. 31, 208–217 (2020).
CAS PubMed Google Scholar
-
Cremoni, M. et al. Th17-immune response in patients with membranous nephropathy is associated with thrombosis and relapses. Front. Immunol. 11, 574997 (2020).
CAS PubMed PubMed Central Google Scholar
-
Motavalli, R. et al. Altered Th17/Treg ratio as a possible mechanism in pathogenesis of idiopathic membranous nephropathy. Cytokine 141, 155452 (2021).
CAS PubMed Google Scholar
-
Rosenzwajg, M. et al. B- and T-cell subpopulations in patients with severe idiopathic membranous nephropathy may predict an early response to rituximab. Kidney Int. 92, 227–237 (2017).
CAS PubMed Google Scholar
-
Cantarelli, C. et al. A comprehensive phenotypic and functional immune analysis unravels circulating anti-phospholipase A2 receptor antibody secreting cells in membranous nephropathy patients. Kidney Int. Rep. 5, 1764–1776 (2020).
PubMed PubMed Central Google Scholar
-
Berchtold, L. et al. HLA-D and PLA2R1 risk alleles associate with recurrent primary membranous nephropathy in kidney transplant recipients. Kidney Int. 99, 671–685 (2021).
CAS PubMed Google Scholar
-
Segerer, S. & Schlondorff, D. B cells and tertiary lymphoid organs in renal inflammation. Kidney Int. 73, 533–537 (2008).
CAS PubMed Google Scholar
-
Kolovou, K. et al. B-cell oligoclonal expansions in renal tissue of patients with immune-mediated glomerular disease. Clin. Immunol. 217, 108488 (2020).
CAS PubMed Google Scholar
-
Prunotto, M. et al. Proteomic analysis of podocyte exosome-enriched fraction from normal human urine. J. Proteom. 82, 193–229 (2013).
CAS Google Scholar
-
Kerjaschki, D. & Neale, T. J. Molecular mechanisms of glomerular injury in rat experimental membranous nephropathy (Heymann nephritis). J. Am. Soc. Nephrol. 7, 2518–2526 (1996).
CAS PubMed Google Scholar
-
Huang, C. C. et al. IgG subclass staining in renal biopsies with membranous glomerulonephritis indicates subclass switch during disease progression. Mod. Pathol. 26, 799–805 (2013).
CAS PubMed Google Scholar
-
Val-Bernal, J. F., Garijo, M. F., Val, D., Rodrigo, E. & Arias, M. C4d immunohistochemical staining is a sensitive method to confirm immunoreactant deposition in formalin-fixed paraffin-embedded tissue in membranous glomerulonephritis. Histol. Histopathol. 26, 1391–1397 (2011).
CAS PubMed Google Scholar
-
Hayashi, N. et al. Glomerular mannose-binding lectin deposition in intrinsic antigen-related membranous nephropathy. Nephrol. Dial. Transplant. 33, 832–840 (2018).
CAS PubMed Google Scholar
-
Bally, S. et al. Phospholipase A2 receptor-related membranous nephropathy and mannan-binding lectin deficiency. J. Am. Soc. Nephrol. 27, 3539–3544 (2016).
PubMed PubMed Central Google Scholar
-
Ravindran, A. et al. Proteomic analysis of complement proteins in membranous nephropathy. Kidney Int. Rep. 5, 618–626 (2020).
PubMed PubMed Central Google Scholar
-
Cybulsky, A. V., Quigg, R. J. & Salant, D. J. Experimental membranous nephropathy redux. Am. J. Physiol. Ren. Physiol. 289, F660–F671 (2005).
CAS Google Scholar
-
Tomas, N. M. et al. Autoantibodies against thrombospondin type 1 domain-containing 7A induce membranous nephropathy. J. Clin. Invest. 126, 2519–2532 (2016).
PubMed PubMed Central Google Scholar
-
Tomas, N. M. et al. A heterologous model of thrombospondin type 1 domain-containing 7A-associated membranous nephropathy. J. Am. Soc. Nephrol. 28, 3262–3277 (2017).
CAS PubMed PubMed Central Google Scholar
-
Petrosyan, A. et al. A glomerulus-on-a-chip to recapitulate the human glomerular filtration barrier. Nat. Commun. 10, 3656 (2019).
PubMed PubMed Central Google Scholar
-
Haddad, G. et al. Altered glycosylation of IgG4 promotes lectin complement pathway activation in anti-PLA2R1 associated membranous nephropathy. J. Clin. Invest. 131, e140453 (2021). This article provides the first demonstration of the pathogenic role of modified IgG4 specific for PLA2R in lectin pathway activation.
CAS PubMed Central Google Scholar
-
Ghiggeri, G. M. et al. Multi-autoantibody signature and clinical outcome in membranous nephropathy. Clin. J. Am. Soc. Nephrol. 15, 1762–1776 (2020).
PubMed PubMed Central Google Scholar
-
Seikrit, C., Ronco, P. & Debiec, H. Factor H autoantibodies and membranous nephropathy. N. Engl. J. Med. 379, 2479–2481 (2018).
PubMed Google Scholar
-
Barbour, S. J. et al. Disease-specific risk of venous thromboembolic events is increased in idiopathic glomerulonephritis. Kidney Int. 81, 190–195 (2012).
PubMed Google Scholar
-
Kerlin, B. A., Ayoob, R. & Smoyer, W. E. Epidemiology and pathophysiology of nephrotic syndrome-associated thromboembolic disease. Clin. J. Am. Soc. Nephrol. 7, 513–520 (2012).
CAS PubMed PubMed Central Google Scholar
-
Lionaki, S. et al. Venous thromboembolism in patients with membranous nephropathy. Clin. J. Am. Soc. Nephrol. 7, 43–51 (2012).
CAS PubMed Google Scholar
-
Cattran D. C. et al. (eds) National Kidney Foundation’s Primer on Kidney Diseases 7th Edn 188–197 (Elsevier, 2018).
-
Agrawal, S., Zaritsky, J. J., Fornoni, A. & Smoyer, W. E. Dyslipidaemia in nephritic syndrome: mechanisms and treatment. Nat. Rev. Nephrol. 14, 57–70 (2018).
CAS PubMed Google Scholar
-
Rodriguez, E. F. et al. Membranous nephropathy with crescents: a series of 19 cases. Am. J. Kidney Dis. 64, 66–73 (2014).
PubMed Google Scholar
-
Fogo, A. B., Lusco, M. A., Najafian, B. & Alpers, C. E. Atlas of renal pathology: membranous nephropathy. Am. J. Kidney Dis. 66, e43–e45 (2015).
PubMed Google Scholar
-
Beck, L. H., Fervenza, F. C. In Molecular Mechanisms in the Pathogenesis of Idiopathic Nephrotic Syndrome (ed. Kaneko, K.) 181–205 (Springer Japan, 2016).
-
Markowitz, G. S. Membranous glomerulopathy: emphasis on secondary forms and disease variants. Adv. Anat. Pathol. 8, 119–125 (2001).
CAS PubMed Google Scholar
-
Kuroki, A. et al. Glomerular and serum IgG subclasses in diffuse proliferative lupus nephritis, membranous lupus nephritis, and idiopathic membranous nephropathy. Intern. Med. 41, 936–942 (2002).
CAS PubMed Google Scholar
-
Ronco, P., Plaisier, E. & Debiec, H. Advances in membranous nephropathy. J. Clin. Med. 10, 607 (2021).
CAS PubMed PubMed Central Google Scholar
-
Qu, Z. et al. Absence of glomerular IgG4 deposition in patients with membranous nephropathy may indicate malignancy. Nephrol. Dial. Transplant. 27, 1931–1937 (2012).
CAS PubMed Google Scholar
-
von Haxthausen, F. et al. Antigen-specific IgG subclasses in primary and malignancy-associated membranous nephropathy. Front. Immunol. 9, 3035 (2018).
Google Scholar
-
van de Logt, A. E., Hofstra, J. M. & Wetzels, J. F. Serum anti-PLA2R antibodies can be initially absent in idiopathic membranous nephropathy: seroconversion after prolonged follow-up. Kidney Int. 87, 1263–1264 (2015).
PubMed Google Scholar
-
Debiec, H. & Ronco, P. PLA2R autoantibodies and PLA2R glomerular deposits in membranous nephropathy. N. Engl. J. Med. 364, 689–690 (2011).
CAS PubMed Google Scholar
-
Svobodova, B., Honsova, E., Ronco, P., Tesar, V. & Debiec, H. Kidney biopsy is a sensitive tool for retrospective diagnosis of PLA2R-related membranous nephropathy. Nephrol. Dial. Transplant. 28, 1839–1844 (2013).
CAS PubMed Google Scholar
-
Luo, J., Zhang, W., Su, C., Zhou, Z. & Wang, G. Seropositive PLA2R-associated membranous nephropathy but biopsy-negative PLA2R staining. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfaa239 (2020).
Article PubMed PubMed Central Google Scholar
-
Poggio, E. D. et al. Systematic review and meta-analysis of native kidney biopsy complications. Clin. J. Am. Soc. Nephrol. 15, 1595–1602 (2020).
PubMed PubMed Central Google Scholar
-
Pombas, B. et al. Risk factors associated with major complications after ultrasound-guided percutaneous renal biopsy of native kidneys. Kidney Blood. Press. Res. 45, 122–130 (2020).
PubMed Google Scholar
-
Palsson, R. et al. Bleeding complications after percutaneous native kidney biopsy: results from the Boston Kidney Biopsy cohort. Kidney Int. Rep. 5, 511–518 (2020).
PubMed PubMed Central Google Scholar
-
Atwell, T. D. et al. The timing and presentation of major hemorrhage after 18,947 image-guided percutaneous biopsies. Am. J. Roentgenol. 205, 190–195 (2015).
Google Scholar
-
Bobart, S. A. et al. Noninvasive diagnosis of primary membranous nephropathy using phospholipase A2 receptor antibodies. Kidney Int. 95, 429–438 (2019).
CAS PubMed Google Scholar
-
Bobart, S. A. et al. Kidney biopsy is required for nephrotic syndrome with PLA2R+ and normal kidney function: the Con View. Kidney 360, 890–893 (2020).
Google Scholar
-
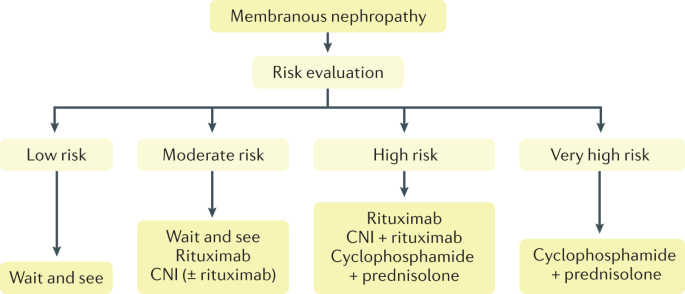
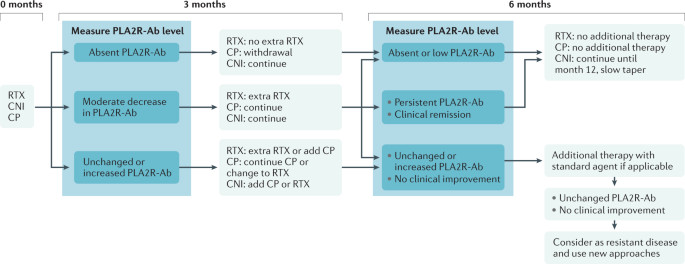
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int. 100, S1–S276 (2021). A milestone for the management of glomerular diseases.
-
Bobart, S. A. et al. A target antigen-based approach to the classification of membranous nephropathy. Mayo Clin. Proc. 96, 577–591 (2021).
CAS PubMed Google Scholar
-
Larsen, C. P. et al. Determination of primary versus secondary membranous glomerulopathy utilizing phospholipase A2 receptor staining in renal biopsies. Mod. Pathol. 26, 709–715 (2013).
CAS PubMed Google Scholar
-
Stehle, T. et al. Phospholipase A2 receptor and sarcoidosis-associated membranous nephropathy. Nephrol. Dial. Transplant. 30, 1047–1050 (2015).
CAS PubMed Google Scholar
-
Xie, Q. et al. Renal phospholipase A2 receptor in hepatitis B virus-associated membranous nephropathy. Am. J. Nephrol. 41, 345–353 (2015).
CAS PubMed Google Scholar
-
Berchtold, L. et al. Efficacy and safety of rituximab in hepatitis B virus-associated PLA2R-positive membranous nephropathy. Kidney Int. Rep. 3, 486–491 (2018).
PubMed Google Scholar
-
Qin, W. et al. Anti-phospholipase A2 receptor antibody in membranous nephropathy. J. Am. Soc. Nephrol. 22, 1137–1143 (2011).
CAS PubMed PubMed Central Google Scholar
-
Hanset, N. et al. Podocyte antigen staining to identify distinct phenotypes and outcomes in membranous nephropathy: a retrospective multicenter cohort study. Am. J. Kidney Dis. 76, 624–635 (2020).
CAS PubMed Google Scholar
-
Zhang, Z. et al. Duodenal schwannoma as a rare association with membranous nephropathy: a case report. Am. J. Kidney Dis. 73, 278–280 (2019).
PubMed Google Scholar
-
Zaghrini, C. et al. Novel ELISA for thrombospondin type 1 domain-containing 7A autoantibodies in membranous nephropathy. Kidney Int. 95, 666–679 (2019).
CAS PubMed Google Scholar
-
Sharma, S. G. & Larsen, C. P. Tissue staining for THSD7A in glomeruli correlates with serum antibodies in primary membranous nephropathy: a clinicopathological study. Mod. Pathol. 31, 616–622 (2018).
CAS PubMed Google Scholar
-
Schlumberger, W. et al. Differential diagnosis of membranous nephropathy with autoantibodies to phospholipase A2 receptor 1. Autoimmun. Rev. 13, 108–113 (2014).
CAS PubMed Google Scholar
-
Timmermans, S. A. et al. Evaluation of anti-PLA2R1 as measured by a novel ELISA in patients with idiopathic membranous nephropathy: a cohort study. Am. J. Clin. Pathol. 142, 29–34 (2014).
PubMed Google Scholar
-
Liu, Y. et al. Serum anti-PLA2R antibody as a diagnostic biomarker of idiopathic membranous nephropathy: the optimal cut-off value for Chinese patients. Clin. Chim. Acta 476, 9–14 (2018).
CAS PubMed Google Scholar
-
Behnert, A. et al. Antiphospholipase A2 receptor autoantibodies: a comparison of three different immunoassays for the diagnosis of idiopathic membranous nephropathy. J. Immunol. Res. 2014, 143274 (2014).
PubMed PubMed Central Google Scholar
-
Pourcine, F. et al. Prognostic value of PLA2R autoimmunity detected by measurement of anti-PLA2R antibodies combined with detection of PLA2R antigen in membranous nephropathy. A single-centre study over 14 years. PLoS ONE 12, e0173201 (2017).
PubMed PubMed Central Google Scholar
-
Plaisier, E. & Ronco, P. Screening for cancer in patients with glomerular diseases. Clin. J. Am. Soc. Nephrol. 15, 886–888 (2020).
CAS PubMed PubMed Central Google Scholar
-
Cambier, J. F. & Ronco, P. Onco-nephrology: glomerular diseases with cancer. Clin. J. Am. Soc. Nephrol. 7, 1701–1712 (2012).
CAS PubMed Google Scholar
-
Timmermans, S. A. et al. Anti-phospholipase A2 receptor antibodies and malignancy in membranous nephropathy. Am. J. Kidney Dis. 62, 1223–1225 (2013).
CAS PubMed Google Scholar
-
Wang, G. et al. Neural epidermal growth factor-Like 1 protein-positive membranous nephropathy in Chinese patients. Clin. J. Am. Soc. Nephrol. 8, 727–735 (2021).
Google Scholar
-
Ayalon, R. & Beck, L. H. Jr Membranous nephropathy: not just a disease for adults. Pediatr. Nephrol. 30, 31–39 (2015).
PubMed Google Scholar
-
Debiec, H., Ronco, P. & Vivarelli, M. Congenital membranous nephropathy due to fetomaternal anti-neutral endopeptidase alloimmunization. Orphanet https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=69063 (2020).
-
Bhimma, R. & Coovadia, H. M. Hepatitis B virus-associated nephropathy. Am. J. Nephrol. 24, 198–211 (2004).
CAS PubMed Google Scholar
-
Safar-Boueri, L., Piya, A., Beck, L. H. Jr & Ayalon, R. Membranous nephropathy: diagnosis, treatment, and monitoring in the post-PLA2R era. Pediatr. Nephrol. 36, 19–30 (2021).
PubMed Google Scholar
-
Debiec, H. et al. Allo-immune membranous nephropathy and recombinat arylsulfatase replacement therapy: a need for tolerance induction therapy. J. Am. Soc. Nephrol. 25, 675–680 (2014).
CAS PubMed Google Scholar
-
Wang, R. et al. Long-term renal survival and related risk factors for primary membranous nephropathy in Chinese children: a retrospective analysis of 217 cases. J. Nephrol. 34, 589–596 (2021).
CAS PubMed Google Scholar
-
Ramachandran R. & Jha, V. in Glomerulonephritis (eds Trachtman H., Hogan J. J., Herlitz L. & Lerma E. V.) (Springer, 2020).
-
Htay, H. et al. Global access of patients with kidney disease to health technologies and medications: findings from the Global Kidney Health Atlas project. Kidney Int. Suppl. 8, 64–73 (2018).
Google Scholar
-
Hepatitis B Foundation. World Health Organization. Addressing Hepatitis B in Africa. Hepatitis B Foundation https://www.hepb.org/blog/addressing-hepatitis-b-africa/ (2020).
-
Kumar, M. N. et al. Membranous nephropathy associated with indigenous Indian medications containing heavy metals. Kidney Int. Rep. 5, 1510–1514 (2020).
PubMed PubMed Central Google Scholar
-
Landrigan, P. J. et al. The Lancet Commission on pollution and health. Lancet 391, 462–512 (2018).
PubMed Google Scholar
-
Gupta, S., Pepper, R. J., Ashman, N. & Walsh, S. B. Nephrotic syndrome: oedema formation and its treatment with diuretics. Front. Physiol. 9, 1868 (2019).
PubMed PubMed Central Google Scholar
-
Hinrichs, G. R., Jensen, B. L. & Svenningsen, P. Mechanisms of sodium retention in nephrotic syndrome. Curr. Opin. Nephrol. Hypertens. 29, 207–212 (2020).
CAS PubMed Google Scholar
-
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO clinical practice guideline for glomerulonephritis. Kidney Int. Suppl. 2, 186–197 (2012).
Google Scholar
-
Polanco, N. et al. Spontaneous remission of nephrotic syndrome in idiopathic membranous nephropathy. J. Am. Soc. Nephrol. 2, 697–704 (2020).
Google Scholar
-
Pincus, K. J. & Hynicka, L. M. Prophylaxis of thromboembolic events in patients with nephrotic syndrome. Ann. Pharmacother. 47, 725–734 (2013).
PubMed Google Scholar
-
Medjeral-Thomas, N. et al. Retrospective analysis of a novel regimen for the prevention of venous thromboembolism in nephrotic syndrome. Clin. J. Am. Soc. Nephrol. 9, 478–483 (2014).
PubMed Google Scholar
-
Hofstra, J. M. & Wetzels, J. F. M. Should aspirin be used for primary prevention of thrombotic events in patients with membranous nephropathy? Kidney Int. 89, 981–983 (2016).
CAS PubMed Google Scholar
-
Sexton, D. J. et al. Direct-acting oral anticoagulants as prophylaxis against thromboembolism in the nephrotic syndrome. Kidney Int. Rep. 3, 784–793 (2018).
PubMed PubMed Central Google Scholar
-
Reynolds, M. L., Nachman, P. H., Mooberry, M. J., Crona, D. J. & Derebail, V. K. Recurrent venous thromboembolism in primary membranous nephropathy despite direct Xa inhibitor therapy. J. Nephrol. 32, 669–672 (2019).
CAS PubMed Google Scholar
-
van de Logt, A. E., Hofstra, J. M. & Wetzels, J. F. Pharmacological treatment of primary membranous nephropathy in 2016. Expert Rev. Clin. Pharmacol. 9, 1463–1478 (2016).
PubMed Google Scholar
-
van den Brand, J. A., van Dijk, P. R., Hofstra, J. M. & Wetzels, J. F. Long-term outcomes in idiopathic membranous nephropathy using a restrictive treatment strategy. J. Am. Soc. Nephrol. 25, 150–158 (2014).
PubMed Google Scholar
-
Reichert, L. J., Koene, R. A. & Wetzels, J. F. Prognostic factors in idiopathic membranous nephropathy. Am. J. Kidney Dis. 31, 1–11 (1998).
CAS PubMed Google Scholar
-
Hladunewich, M. A., Troyanov, S., Calafati, J. & Cattran, D. C. Metropolitan Toronto Glomerulonephritis Registry. The natural history of the non-nephrotic membranous nephropathy patient. Clin. J. Am. Soc. Nephrol. 4, 1417–1422 (2009).
PubMed PubMed Central Google Scholar
-
Hoxha, E., Harendza, S., Pinnschmidt, H., Panzer, U. & Stahl, R. A. PLA2R antibody levels and clinical outcome in patients with membranous nephropathy and non-nephrotic range proteinuria under treatment with inhibitors of the renin-angiotensin system. PLoS ONE 9, e110681 (2014).
PubMed PubMed Central Google Scholar
-
Pei, Y., Cattran, D. & Greenwood, C. Predicting chronic renal insufficiency in idiopathic membranous glomerulonephritis. Kidney Int. 42, 960–966 (1992).
CAS PubMed Google Scholar
-
Howman, A. et al. Immunosuppression for progressive membranous nephropathy: a UK randomised controlled trial. Lancet 381, 744–751 (2013).
CAS PubMed PubMed Central Google Scholar
-
Cattran, D. C. et al. Validation of a predictive model of idiopathic membranous nephropathy: its clinical and research implications. Kidney Int. 51, 901–907 (1997).
CAS PubMed Google Scholar
-
van den Brand, J. A., Hofstra, J. M. & Wetzels, J. F. Prognostic value of risk score and urinary markers in idiopathic membranous nephropathy. Clin. J. Am. Soc. Nephrol. 7, 1242–1248 (2012).
PubMed PubMed Central Google Scholar
-
van de Logt, A. E. et al. Anti-PLA2R1 antibodies as prognostic biomarker in membranous nephropathy. Kidney Int. Rep. 6, 1677–1686 (2021).
PubMed PubMed Central Google Scholar
-
Lerner, G. B., Virmani, S., Henderson, J. M., Francis, J. M. & Beck, L. H. Jr. A conceptual framework linking immunology, pathology, and clinical features in primary membranous nephropathy. Kidney Int. 100, 289–300 (2021).
CAS PubMed Google Scholar
-
Faul, C. et al. The actin cytoskeleton of kidney podocytes is a direct target of the antiproteinuric effect of cyclosporine A. Nat. Med. 14, 931–938 (2008).
CAS PubMed PubMed Central Google Scholar
-
Ramachandran, R. et al. Two-year follow-up study of membranous nephropathy treated with tacrolimus and corticosteroids versus cyclical corticosteroids and cyclophosphamide. Kidney Int. Rep. 2, 610–616 (2017).
PubMed PubMed Central Google Scholar
-
van de Logt, A. E. et al. Immunological remission in PLA2R-antibody-associated membranous nephropathy: cyclophosphamide versus rituximab. Kidney Int. 93, 1016–1017 (2018).
PubMed Google Scholar
-
Hanset, N. et al. Rituximab in patients with phospholipase A2 receptor-associated membranous nephropathy and severe CKD. Kidney Int. Rep. 5, 331–338 (2019).
PubMed PubMed Central Google Scholar
-
Dahan, K. et al. Retreatment with rituximab for membranous nephropathy with persistently elevated titers of anti-phospholipase A2 receptor antibody. Kidney Int. 95, 233–234 (2019).
CAS PubMed Google Scholar
-
van de Logt, A. E. et al. The bias between different albumin assays may affect clinical decision-making. Kidney Int. 95, 1514–1517 (2019).
PubMed Google Scholar
-
Bech, A. P., Hofstra, J. M., Brenchley, P. E. & Wetzels, J. F. Association of anti-PLA2R antibodies with outcomes after immunosuppressive therapy in idiopathic membranous nephropathy. Clin. J. Am. Soc. Nephrol. 9, 1386–1392 (2014).
CAS PubMed PubMed Central Google Scholar
-
Filler, G. et al. Another case of HBV associated membranous glomerulonephritis resolving on lamivudine. Arch. Dis. Child. 88, F154–F156 (2003).
CAS Google Scholar
-
O’Shaughnessy, M. M. et al. Treatment patterns among adults and children with membranous nephropathy in the Cure Glomerulonephropathy Network (CureGN). Kidney Int. Rep. 4, 1725–1734 (2019).
PubMed PubMed Central Google Scholar
-
Riaz, P. et al. Workforce capacity for the care of patients with kidney failure across world countries and regions. BMJ Glob. Health 6, e004014 (2021).
PubMed PubMed Central Google Scholar
-
Jha, V. et al. Understanding kidney care needs and implementation strategies in low- and middle-income countries: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) controversies conference. Kidney Int. 90, 1164–1174 (2016).
PubMed Google Scholar
-
Cosio, F. G. & Cattran, D. C. Recent advances in our understanding of recurrent primary glomerulonephritis after kidney transplantation. Kidney Int. 91, 304–314 (2017).
PubMed Google Scholar
-
Grupper, A. et al. Recurrent membranous nephropathy after kidney transplantation: treatment and long-term implications. Transplantation 100, 2710–2716 (2016).
CAS PubMed Google Scholar
-
Seitz-Polski, B. et al. Prediction of membranous nephropathy recurrence after transplantation by monitoring of anti-PLA2R1 (M-type phospholipase A2 receptor) autoantibodies: a case series of 15 patients. Nephrol. Dial. Transplant. 29, 2334–2342 (2014).
CAS PubMed Google Scholar
-
Quintana, L. F. et al. Antiphospholipase A2 receptor antibody levels predict the risk of posttransplantation recurrence of membranous nephropathy. Transplantation 99, 1709–1714 (2015).
CAS PubMed Google Scholar
-
Andrésdóttir, M. B. & Wetzels, J. F. Increased risk of recurrence of membranous nephropathy after related donor kidney transplantation. Am. J. Transplant. 12, 265–266 (2012).
PubMed Google Scholar
-
Gupta, G. et al. Pre-transplant phospholipase A2 receptor autoantibody concentration is associated with clinically significant recurrence of membranous nephropathy post-kidney transplantation. Clin. Transplant. 30, 461–469 (2016).
CAS PubMed Google Scholar
-
Batal, I. et al. Association of HLA typing and alloimmunity with posttransplantation membranous nephropathy: a multicenter case series. Am. J. Kidney Dis. 76, 374–383 (2020).
CAS PubMed PubMed Central Google Scholar
-
Kattah, A. et al. Anti-phospholipase A2 receptor antibodies in recurrent membranous nephropathy. Am. J. Transplant. 15, 1349–1359 (2015).
CAS PubMed PubMed Central Google Scholar
-
WHO. Programme on Mental Health. WHOQOL User Manual (World Health Organization, 1998).
-
Wyld, M., Morton, R. L., Hayen, A., Howard, K. & Webster, A. C. A systematic review and meta-analysis of utility-based quality of life in chronic kidney disease treatments. PLoS Med. 9, e1001307 (2012).
PubMed PubMed Central Google Scholar
-
Chuasuwan, A., Pooripussarakul, S., Thakkinstian, A., Ingsathit, A. & Pattanaprateep, O. Comparisons of quality of life between patients underwent peritoneal dialysis and hemodialysis: a systematic review and meta-analysis. Health Qual. Life. Outcomes 18, 191 (2020).
PubMed PubMed Central Google Scholar
-
Canetta, P. A. et al. Health-related quality of life in glomerular disease. Kidney Int. 95, 1209–1224 (2019).
PubMed PubMed Central Google Scholar
-
Cattran, D. Management of membranous nephropathy: when and what for treatment. J. Am. Soc. Nephrol. 16, 1188–1194 (2005).
PubMed Google Scholar
-
Libório, A. B. et al. Proteinuria is associated with quality of life and depression in adults with primary glomerulopathy and preserved renal function. PLoS ONE 7, e37763 (2012).
PubMed PubMed Central Google Scholar
-
Floege, J. et al. Management and treatment of glomerular diseases (part 1): conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) controversies conference. Kidney Int. 95, 268–280 (2019).
PubMed Google Scholar
-
Murphy, S. L. et al. Longitudinal changes in health-related quality of life in primary glomerular disease: results from the CureGN study. Kidney Int. Rep. 5, 1679–1689 (2020).
PubMed PubMed Central Google Scholar
-
Center for Drug Evaluation and Research, Center for Devices and Radiological Health and Center for Biologics Evaluation and Research. Guidance for Industry. Patient-Reported Outcome Measures: Use in Medical Product Development To Support Labeling Claims (FDA, 2009).
-
Bansal, D., Bhagat, A., Schifano, F. & Gudala, K. Role of patient-reported outcomes and other efficacy endpoints in the drug approval process in Europe (2008-2012). J. Epidemiol. Glob. Health 5, 385–395 (2015).
PubMed PubMed Central Google Scholar
-
Carter, S. A. et al. Identifying outcomes important to patients with glomerular disease and their caregivers. Clin. J. Am. Soc. Nephrol. 15, 673–684 (2020).
PubMed PubMed Central Google Scholar
-
Henkel, C. & Hoffmann, P. (Eds) MALDI Imaging. Biochim. Biophys. Acta 1865, 725–978 (2017).
Google Scholar
-
Neumann, E. K., Djambazova, K. V., Caprioli, R. M. & Spraggins, J. M. Multimodal imaging mass spectrometry: next generation molecular mapping in biology and medicine. J. Am. Soc. Mass. Spectrom. 31, 2401–2415 (2020).
CAS PubMed Google Scholar
-
Unnersjö-Jess, D., Scott, L., Blom, H. & Brismar, H. Super-resolution stimulated emission depletion imaging of slit diaphragm proteins in optically cleared kidney tissue. Kidney Int. 89, 243–247 (2016).
PubMed Google Scholar
-
Park, J., Liu, C. L., Kim, J. & Susztak, K. Understanding the kidney one cell at a time. Kidney Int. 96, 862–870 (2019).
CAS PubMed PubMed Central Google Scholar
-
Ellebrecht, C. T. et al. Reengineering chimeric antigen receptor T cells for targeted therapy of autoimmune disease. Science 353, 179–184 (2016).
CAS PubMed PubMed Central Google Scholar
-
Wraith, D. Autoimmunity: antigen-specific immunotherapy. Nature 530, 422–423 (2016).
CAS PubMed Google Scholar
-
Abedini, A. et al. Urinary single-cell profiling captures the cellular diversity of the kidney. J. Am. Soc. Nephrol. 32, 614–627 (2021).
CAS PubMed PubMed Central Google Scholar
-
Unlu, G. et al. GRIK5 genetically regulated expression associated with eye and vascular phenomes: discovery through iteration among biobanks, electronic health records, and Zebrafish. Am. J. Hum. Genet. 104, 503–519 (2019).
CAS PubMed PubMed Central Google Scholar
-
Reddy, V. et al. Obinutuzumab induces superior B-cell cytotoxicity to rituximab in rheumatoid arthritis and systemic lupus erythematosus patient samples. Rheumatology 56, 1227–1237 (2017).
CAS PubMed PubMed Central Google Scholar
-
Klomjit, N., Fervenza, F. C. & Zand, L. Successful treatment of patients with refractory PLA2 R-associated membranous nephropathy with obinutuzumab: a report of 3 cases. Am. J. Kidney Dis. 76, 883–888 (2020).
CAS PubMed Google Scholar
-
Podestà, M. A., Ruggiero, B., Remuzzi, G. & Ruggenenti, P. Ofatumumab for multirelapsing membranous nephropathy complicated by rituximab-induced serum- sickness. BMJ Case. Rep. 13, e232896 (2020).
PubMed PubMed Central Google Scholar
-
Schmidt, T., Schulze, M., Harendza, S. & Hoxha, E. Successful treatment of PLA2R1-antibody positive membranous nephropathy with ocrelizumab. J. Nephrol. 34, 603–606 (2021).
CAS PubMed Google Scholar
-
Samy, E., Wax, S., Huard, B., Hess, H. & Schneider, P. Targeting BAFF and APRIL in systemic lupus erythematosus and other antibody-associated diseases. Int. Rev. Immunol. 36, 3–19 (2017).
CAS PubMed Google Scholar
-
Mahévas, M. et al. Efficacy, safety and immunological profile of combining rituximab with belimumab for adults with persistent or chronic immune thrombocytopenia: results from a prospective phase 2b trial. Haematologica https://doi.org/10.3324/haematol.2020.259481 (2020).
Article PubMed Central Google Scholar
-
Furie, R. et al. Two-year, randomized, controlled trial of belimumab in lupus nephritis. N. Engl. J. Med. 383, 1117–1128 (2020).
CAS PubMed Google Scholar
-
Barrett, C. et al. Effect of belimumab on proteinuria and anti-phospholipase A2 receptor autoantibody in primary membranous nephropathy. Nephrol. Dial. Transplant. 35, 599–606 (2020).
CAS PubMed Google Scholar
-
Crickx, E., Weill, J. C., Reynaud, C. A. & Mahévas, M. Anti-CD20-mediated B-cell depletion in autoimmune diseases: successes, failures and future perspectives. Kidney Int. 97, 885–893 (2020).
CAS PubMed Google Scholar
-
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04145440 (2021).
-
Weinmann-Menke, J. et al. Treatment of membranous nephropathy in patients with THSD7A antibodies using immunoadsorption. Am. J. Kidney Dis. 74, 849–852 (2019).
CAS PubMed Google Scholar
-
Podestà, M. A. et al. Accelerating the depletion of circulating anti-phospholipase A2 receptor antibodies in patients with severe membranous nephropathy: preliminary findings with double filtration plasmapheresis and ofatumumab. Nephron 144, 30–35 (2020).
PubMed Google Scholar
-
Zipfel, P. F. et al. Complement inhibitors in clinical trials for glomerular diseases. Front. Immunol. 10, 2166 (2019).
CAS PubMed PubMed Central Google Scholar
-
Low, J. H. et al. Generation of human PSC-derived kidney organoids with patterned nephron segments and a de novo vascular network. Cell Stem. Cell 25, 373–387 (2019).
CAS PubMed PubMed Central Google Scholar
-
Maas, R. J. et al. Kidney injury molecule-1 and neutrophil gelatinase-associated lipocalin as prognostic markers in idiopathic membranous nephropathy. Ann. Clin. Biochem. 53, 51–57 (2016).
CAS PubMed Google Scholar
-
van den Brand, J. A., Hofstra, J. M. & Wetzels, J. F. Low-molecular-weight proteins as prognostic markers in idiopathic membranous nephropathy. Clin. J. Am. Soc. Nephrol. 6, 2846–2853 (2011).
PubMed PubMed Central Google Scholar